Catch up on these posts here first if you missed any part of the birth story:
34w5d: I get a cervical dilation
I was admitted at 12:05 am October 2 and discharged October 12. I spent 11 days in the hospital.
The trauma surrounding my hospitalization with Olivia’s birth stuck with me for a long time. I wanted a different experience with this birth. And I did. I mean a lot of good things happened with Emelia’s birth. I got my VBAC. The birth itself was so empowering. So incredibly empowering. I was in control. My birth plan was followed. I couldn’t have asked for a better doctor. And even postpartum, there were a lot of good things that happened that didn’t happen with Olivia’s birth.
First, my blood pressure stabilized much more quickly than it did with Olivia. With Olivia, it took six days for the on-call doctors to find a medication combination that would stabilize my pressures. Who knows how many docs had a hand in my chart, following their freaking protocols until I had to outright refuse treatment and forced the nurse to call the on-call OB back to try something else, something outside his freaking protocol.
This time around, my doctor was able to stabilize it in three days.
On the day I gave birth to Emelia, my pressures started skyrocketing. I was on labetalol twice a day and had an as-needed med, Procardia, for when my BP went over 160/100. It was only this med that ever brought my numbers down, to that perfect 120/80.
On postpartum day 1, we went to labetalol three times a day and it did nothing. That afternoon I ran into my nurse coming into my room and she told me my doctor was going to come see me, but that he’s nixing the labetalol and finding something else. When I talked to him later, he told me he didn’t think the labetalol was doing anything so he got rid of it for an extended-release Procardia and a med called Aldomet. It was this combination that stabilized everything by postpartum day 2. What kept me in the hospital for another four days was elevated liver enzymes. Unfortunately, a side effect of Aldomet is elevated liver enzymes. So while initially, my labs were going down, they rose again once I started the Aldomet. Was this a side effect or the preeclampsia returning? He was hesitant to send me home until he saw a decrease because if this was preeclampsia returning, he didn’t want me to come back to the hospital after I was discharged. I didn’t want that either.
I was on magnesium until 6:00 am the morning after Emelia was born. Finally getting free of all wires and tubes was indescribable. I could walk to the bathroom without a whole spectacle of unplugging two different cords from the wall, and dragging an IV pole with me. I could see straight without thinking I was drunk. Magnesium sucks and I was worried I would have to go back on it.
The day Emelia was born, I visited her three times. When my blood pressure finally stabilized (on that as-needed wonder drug) and I could finally go down there, it had been about three hours since she had been born. Chris was sending me photos, commenting on how much she looked like Olivia. He finger fed her the colostrum. And I remember crying in bed, my blood pressure cuff attached to my arm as I waited for another check, seeing the resemblance to my other daughter and feeling like I was missing out on something really crucial.
The neonatal nurse practitioner came to see me during that time to give me an update. She was stable. But no, my husband couldn’t hold her because she had had that apneic event after birth and she needed to make sure Emelia didn’t have another episode again before we could hold her. I cried again when she left.
My blood pressure finally went down to something like 140/90 and I was placed in a wheelchair and wheeled down to her. Since the NICU was full, she was over in the back corner in her warmer hanging out until a baby discharged so she could take their place. I wheeled up to her and put my hand on her. She was little and asleep. They had placed an IV. I asked the nurse if I could do skin and to skin and she said of course.
Later that evening, my blood pressure didn’t cooperate again. Chris had to go down to see her without me, while I waited again for it to go down (I needed the Procardia again).
Tell her Mama’s sorry she can’t be there once again, I texted Chris.
I wish they would just bring you down here. Keeping you in the bed isn’t helping you out, he texted back.
I’m so scared she’s not going to be able to bond with me with how much I can’t be with her.
She’s going to bond with you. Don’t worry about that. She knows who her mama is.
Monday, October 7: We start bottle-feeds
Postpartum day 1 was insane. It was more of the same, with something going on with me at the moment I wanted to go visit Emelia, so Chris was sent down ahead of me. I showered for the first time since giving birth while Chris left to get breakfast. While waiting for the nurse, I pumped, ate breakfast, and then met with lactation, and after that, my doula.
“I feel like there’s so much going on,” I told her. “Like, I’m not really thinking too much into things, and I’m not even really feeling anything.”
“You’re on survival mode,” she told me, “And it’s perfectly OK to get through this and deal with the trauma when you get home. It’s OK right now not to feel anything.”
It became my mantra. Don’t stop, don’t think.
Don’t stop. Don’t think.
That’s how I’m getting through this.
Don’t stop, don’t think.
Don’t cry because you won’t stop.
Don’t breakdown because you don’t have time for that right now.
This little girl is so amazing.
But it was still so fucking hard.
I did another assessment with the nurse. I met with Integrative Medicine for a foot and hand massage. I finally got some time to get down to the NICU before needing to go back again to eat lunch. And then my blood pressure was high again.
My mom came in the afternoon to see Emelia. I had to pump again. And so began a ritual. I was assessed by nurses. I pumped and ordered breakfast. I waited for what seemed like ages for my blood pressure to go down before I saw the baby. I met with lactation or my doctor or both. I pumped. I saw the baby. I ate. I pumped. I tried to get in one to two sitz baths a day.
Emelia was on TPN (nutrition given through an IV) and Chris talked to her medical team in rounds about how we as her parents had no idea she was started on this. That we felt like we weren’t involved in her care as we should be. The magnesium had affected her like it was affecting me and she was very sleepy and pretty much out of it, so they wanted to make sure she was alert enough to take in a bottle.
The staff apologized and told us they’d be updating us regularly. She started oral feeds at 10mLs, and slowly advanced. What I couldn’t produce for her was supplemented with donor milk. She was more awake that day and did a great job eating.
I did skin to skin with her as much as I could. It never felt like it was enough.
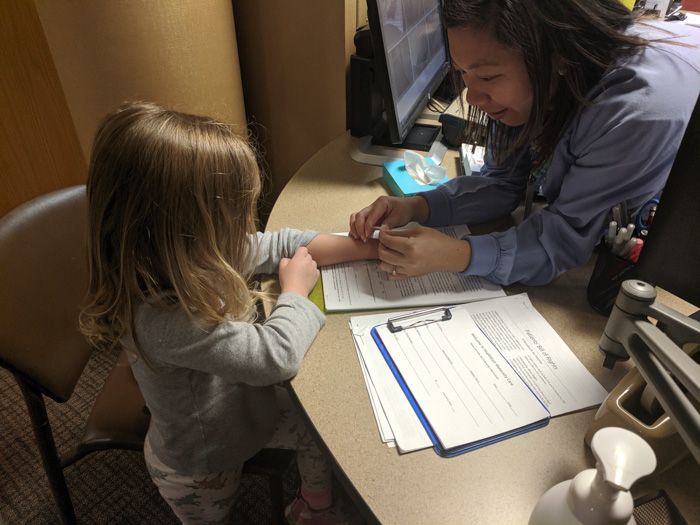
The lactation consultant checked her for ties and declared her palate “beautiful!” She had a strong suck. I was encouraged to let her hang out by my breasts and let her try latching, but not to force anything. They had to restart her IV because the first one went bad. Everyone was hoping this one would stay in until she didn’t need the IV fluids because she was a hard stick and they didn’t want to put her through another one.
Don’t stop, don’t think.
We talked to Olivia on the phone that evening. My mom said she was just having a hard time and thought we could say goodnight to her. I had been in the hospital for 6 days. We asked her about her day and what she ate for dinner. And then—
“Mama, I want you to come home.” Her voice cracked and I knew she was tearing up.
I lost it. I could barely finish talking to her, so Chris took over. And then I had my first hospital meltdown.
I had one child in the NICU that couldn’t sleep next to me. I had to plan my visits to her around everything else I had going on. I had one child crying for me because she didn’t understand what was taking so long for me to come home. She didn’t know she had a sister because I wasn’t sure how to explain that we weren’t all coming home as a family when I told her we would. I couldn’t prepare her for all this.
I was exhausted by the time I went to bed.
Tuesday, October 8: Olivia meets her sister
Things were becoming a blur. The shifts were starting to run together and I couldn’t even remember my nurses’ names anymore because I had them for a few hours and never saw them again.
Emelia latched and nursed for about 30 seconds with the help of her nurse. It was amazing.
We decided to have my parents come up to the hospital that evening with Olivia and tell her she was a big sister. They came and she sat on my hospital bed (she wondered why I didn’t have my super awesome IV anymore) and I told her that Mama had the baby. No, she isn’t here because sometimes when babies are born they have to be in the baby room for a little bit, but we can go down to see her. And yes, sometimes Mamas have to stay in the hospital for a little bit after they have their babies. She seemed to take all this in stride. We gave Olivia a present that her little sister got her and told her her sister’s name was Emelia. She was so excited.
Since the NICU nurses were doing report, we had to wait until 7:30 to get in, so we talked to my parents while Olivia and I played on the bed.
When it was time, we walked to the front desk and Olivia got to pick out a Big Sister bracelet.
Then we walked down to the Baby Room to see her sister.
It wasn’t the meeting I was wanting. But it was still pretty good. Olivia was perfect. She used her quiet voice and was so gentle with her sister.
It was hard with the alarms constantly beeping and every once in awhile she’d glance over at the monitor and the wires.
She got to give Emelia the stuffed bear she had picked out and explained to her (much to the nurse’s amusement) that her name is Emelia, but she was Queso inside Mama.
There was one moment when Emelia’s sats dropped down to 80 and even into the 70s before rising again. The nurse said later she was looking a little dusky in her face, so that was another event we were hoping she wouldn’t have again. She thought maybe it was overstimulation being held by Olivia. That was hard to hear.
My dad came in for a few minutes to meet her (I have zero pictures of my parents holding her in the NICU because I suck), and Olivia cried when we told her she had to go back to the room. “I don’t want to leave my sister!”
It was heartbreaking. But I was so glad all of this went well. Even if it wasn’t what I was envisioning.
The evening was hard for me. I had a nurse that was OK-ish who was also training a new nurse. I had forgotten to put in my birth plan that I didn’t want students or new nurses during my stay, and I was feeling myself start to get really annoyed. Everything took longer and that meant delays in getting down to the NICU. And new nurses who were just OK-ish meant I had to start all over. Like, for example, I requested the meds I was taking for sleep while in the hospital, Vistaril and Unisom.
She gave me a confused look and told me they were the thing.
“No, they’re two different medications,” I said. She then proceeded to explain about taking them long term and how they can dry up your milk.
I said not so gently, that if she looked in my chart she’d see I was only taking them while I was here in the hospital. “You guys push me to get sleep, yet you’re in here interrupting me all night. I need something to help.”
After I said goodnight to Emelia, I asked the charge nurse if she’d come to my room. I had her once before and I really liked her. Later, I explained that while most of the nurses were really great, they were all becoming one big blur. As much as possible, I wanted to be assigned the same nurse. She agreed and said she would do her best. I was completely independent now, so I didn’t need much help anymore. We agreed I’d be left alone as much as possible and the nurses would try to group their cares as much as they could. Which ended up going mostly well save for one night later in the week where I had to argue with the nurse (one, of course, I didn’t have before) to figure out how to group her assessment and consolidate her meds with me to maximize my sleep. She wanted to come in at 10, 11, and 1 am for meds and cares and I pushed her to chunk it down.
I needed to get out of this place.
Wednesday, October 9: That really bad day
Wednesday was hard. Emelia had a hard day. She slept most of it, even though she took in her feedings like a champ. She kept de-sating and my anxiety was increasing. On the plus side, her IV was taken out and she lost the appropriate amount of weight, 8%. She was doing great on my colostrum and the donor milk.
But there were a lot of spells and the nurses thought it was related to her positioning, because it wouldn’t happen while she was lying in her crib. The OT who was working with us said day three could be a sleepy day in general.
The nurse assigned to her was not so great. I think she was a good nurse, but… she made the day much harder. She was really serious with us and referred to Emelia as a boy—twice. Chris had told me when I was back in my room that she threatened to put in the NG tube if Emelia didn’t finish her bottle, never mind they were only ten minutes into the feed and she was allotted 30 minutes to finish it. (She ended up finishing it no problem and even a bit more.)
I was holding her skin to skin later that evening when Emelia’s alarms went off, again, for her oxygen sats. I had been glancing nervously up at it throughout the day and worried constantly she was not breathing.
Her nurse came into the room. “It’s time to put her back now,” she told me, pressing some buttons.
“I was just holding her,” I said meekly, as I handed her back.
“Holding her is stressful on her,” she chided, “You should be keeping it to an hour at most.”
I stood next to her crib as the nurse swiftly dressed my baby, tears coming to my eyes. “I was just holding her,” I whispered.
Then I excused myself and walked out, my chest heaving. I kept telling myself not to cry.
Chris followed me back to the room and I ate my forgotten dinner in silence.
“I don’t think I’m going back there tonight,” I told him, starting to cry again, “I guess I just make everything worse.” Yeah, it was a rough day.
Luckily, my nurse that night was someone that actually cared for Emelia in the NICU and I brought up my issues with the nurse there. She told me I can talk to the charge nurse in the NICU and request not to have that nurse back.
Then to make matters worse, that’s the day I also found out my liver enzymes were elevated again. Not enough to treat, my doctor cautioned earlier that day, but we needed to keep an eye on it and retest in the morning. He was anticipating I’d be there through the weekend.
Chris needed to go back home so he could get Olivia to her doctor appointment the next morning. I ended up going back to the NICU after Chris left for the night and luckily the nurse had ended her shift and I had a new nurse for Emelia. I ended up talking to the charge nurse who was really great and she reassured me Emelia wouldn’t have that nurse again.
Back in my room, I realized I had a painful spot on both sides of my breasts. I knew my milk was starting to come in and I made sure I was up pumping when I needed to, but the spots weren’t getting better. It was lonely without Chris, especially dealing with all that.
Thursday, October 10: The NG tube is placed
The next morning, I talked to my nurse about the sore areas. It was a nurse I had before and loved her. The lactation consultant came back and both of them helped me. Apparently, it wasn’t blocked ducts, but rather swelling from all the fluid I had on board from the IV and the preeclampsia. We had to do all sorts of things such as breast lifts (don’t ask, but it felt great) and hand expression.
The neonatologist came in and said they were capping Emelia’s feeds at 45 mL but she can take in more if she wants. She thought the desats were her being tired and having some reflux. The NG tube was there if Emelia wasn’t able to take in all her bottle. If it was placed, it would stay in until discharge so they wouldn’t have to keep replacing it. So far, at four days old, she was still skirting by.
I found out she was moved to the less acute area of the NICU, which was a huge win. She was more alert today and had her eyes open a ton. The lactation consultant came to the NICU and we worked on breastfeeding. She latched on like a champ, but couldn’t maintain it. It was a good session though, enough to poop her out and she wasn’t able to finish the last 18 mLs of her bottle. They needed to place the NG tube. The silver lining, the nurse explained to me, was that now there was no pressure to finish her bottle. That we could do more nursing and they can give her the rest through the tube if she was too tired to finish it.
We did more nursing while the feeds were running, which helped give her the sensation of her belly filling. All in all, it was a much better day, but it was stressful without Chris, since I was still dealing with lots of pumping and having the nurses help with the breast engorgement.
Friday, October 11: Nursing
I heard her crying more today, which meant she was perking up more. This morning she pulled out her NG tube and was feeling pretty smug until her nurse had to put it back in which she did not appreciate. I don’t remember her having any desats.
We nursed twice today, but she can’t maintain a latch. She was a champ at showing interest, opening her mouth wide and rooting around. Her nurses all said the same thing: she’ll get there. Her care team was happy with her feeds. The plan going forward was to nurse her as much as I could while they did the NG tube feeds. When I couldn’t be there, they would give bottles.
Me, I was doing good, considering. At this point, I was basically feeling institutionalized and had no idea how I was going to make it on the outside anymore. I had three meals a day brought to me. I went from my room to the NICU and back again. I was hiding it well, but was feeling more irritable and angry. This just isn’t the way it was supposed to be. And I missed Olivia. Chris was going home again to spend some time with Olivia, so I was alone.
Tomorrow was the day I was hoping to get to go home. I was praying my labs would be going down.
To be continued…



















The pictures of you and Emelia skin to skin, and the pictures of Olivia holding her new baby sister are so precious! I love them! Being in the hospital with a baby in the NICU is rough. It’s SO hard. I remember crying a lot, but I can say they are now a distant memory that I *almost* look back at fondly (if that’s even possible).
You all did so very well. Which sounds odd as obviously things were not what you had hoped for, but your blood pressure did get controlled, you did get some to see and visit your baby and your first child got to visit also. You stood up and walked and were alert and communicated. Best of all, it sounds like your miracle pregnancy is now thriving and you are also. But glory be the process of getting through to this point was not easy. I am so impressed by your clarity of mind and determined efforts in dire situations to get the correct care for you and your child. Such a strong mom. I think your sharing your story is helpful for any future mother, or anyone who knows a mom, who ends up in your situation. Thank you!!!
Your liver enzyme issue makes me wonder if you know if there may be future repercussions from the preeclampsia problems. Please, as you have time and energy, will you research and write about PCOS and preeclampsia impact post pregnancy? You have a gift for making information accessible.
Thank you. AND ABSOLUTE CONGRATULATIONS!!!!!!!!
Aw that all sounds so hard. That one nurse could do with some empathy lessons!
Dang girl. You endured a lot. All the feels for you. Great job advocating for your care!
NICU life is so hard. It’s one of the hardest things I’ve gone through. It felt so foreign to leave my baby lying in an isolatte instead of holding him and having to ask permission to hold your baby or take care of them. It sounds like you did wonderful things to care for Emelia. And yeah….nurses could totally make or break your day.
Oh man- this post brought me back to when Wes was in the NICU and I couldn’t hold him because he was in the bubble and I was so emotional and hormonal. Whew. It is SO HARD. You did a great job mama.
So proud of you girl! And I thought having a baby without going to the ICU was a lot…you are so strong! Emelia is adorable!! Her and Ollie look so alike 🙂 if you need anything please let us know! We know it’s a lot of work going from one to two babies, but even more so after you ling hospital stay! Take care and give both babies some squeezies from us!
The Andress Family,
Kristina, Corey, Kallima, Cayden and doggies